Cognitive therapy gains can be sudden, and can spiral upward
Psychotherapy does not always follow a linear path.
Most… research is based on the assumption that treatment progress in psychotherapy is linear, or log-linear, and follows some form of regular dose-response relationship… However, this assumption regarding the macro, or average level of change, does not necessarily hold for a finer grained analysis of individual progress…
The prevalence of sudden gains found in several studies from different research groups varies between 17% and 50%…
…sudden gains are a phenomenon of cognitive behavioral therapies (CBT) and result from CBT-specific techniques. …substantial cognitive changes could be observed in the therapy session preceding the sudden gains. Sudden gains were followed by a better therapeutic alliance and more cognitive changes in the session after the sudden gain. Thus, the authors postulated an upward spiral, i.e., cognitive changes during the pregain sessions foster the therapeutic alliance and eventually result in additional cognitive changes…
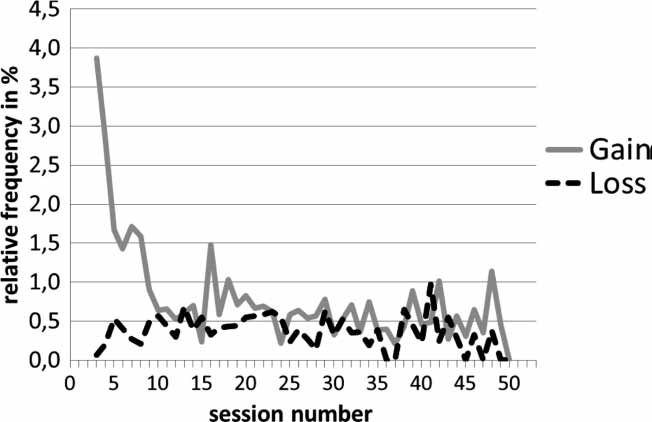
In this paper the frequency of sudden gains as well as sudden losses will be investigated in a large naturalistic outpatient sample (n=1500) with repeated measurements of session progress.
Sudden losses are less frequent, and are more-or-less random
…23.4%… of the patients in the sample experienced at least one sudden gain…
…4.5%… of those experienced a sudden gain and a sudden loss…
…18.9%… had only sudden gains…
…5.47%… experienced only sudden losses.
In contrast to sudden gains, sudden losses occur over the course of treatment without a typical peak of occurrence.
Cognitive therapy gains are greater for people who are hurting more
…those patients who experienced no sudden shifts at all and followed a more linear trajectory had the shortest therapies. At intake patients with no sudden shifts tended to be significantly less disturbed on average… than the three groups with sudden shifts… … post-hoc tests revealed that patients with no sudden shifts were less impaired… compared to sudden gain patients…
…patients with both sudden gains and sudden losses stayed in treatment longer than those in the other groups.
Patients with sudden gains… did not rate the therapeutic relationship significantly higher on average than patients with sudden losses… Results further confirm previous findings that a large amount (about 42%) of sudden gains tend to take place early in therapy and they are part of the phenomenon of early change… But the phenomena also occur later in treatment (about 58%). …we found shorter treatments for patients experiencing sudden gains early in treatment. Patients with early sudden gains showed the highest effect sizes… at the end of treatment.[1]
- Lutz, Wolfgang, et al. “The ups and downs of psychotherapy: Sudden gains and sudden losses identified with session reports.” Psychotherapy Research 23.1 (2013): 14-24.