[1]
Psychiatric medication development declined steeply after the 1950s and 1960s
…there has been a steep decline in the development of new medication classes. Instead of new molecular entities, slight molecular modifications producing ‘‘me-too’’ drugs attempted to garner market share.
The current deficit in novel agents contrasts sharply with the 1950s. Then, there was a sudden efflorescence of potent psychiatric therapeutic agents. The pace of discovery of entirely new classes of psychotropic drugs was dizzying. These included lithium, lysergic acid diethylamide (LSD), chlorpromazine, iproniazid, reserpine, imipramine, chlordiazepoxide, haloperidol, and clozapine.
These discoveries resulted from chance observations of unexpected clinical benefits rather than being derived from basic neuroscience. All major classes were serendipitously discovered by 1969. For instance, chlorpromazine was a pre-surgical antihistamine sedative whose antipsychotic properties were completely unsuspected. Imipramine was developed as a chlorpromazine ‘‘me-too,’’ but turned out to be an antidepressant. Conversely, clozapine was a potential antidepressant, but turned out to be an antipsychotic with remarkably low extrapyramidal toxicity and superior efficacy.
What stymied generative serendipity over the next 40 years? A number of elements came together.
- The most important factor may have been the drastic change in medical practice economics. Hospital-based academic research was supported from clinical income. That freed up clinicians for therapeutic explorations. However, ‘‘managed care’’ declared this irrelevant to patient care and markedly shortened hospital stays.
- Second, often patients were discharged before the effects of a new therapeutic regimen became clear.
- Third, industry became concerned with immediate return on their investments, which were limited by extensive regulations, liability concerns, and exhaustive preclinical animal model testing.
- Fourth, the growth of clinical research organizations (CROs) diverted industrial support from investigator-initiated academic research to relatively inexpensive, pre-set industrial protocols.
Psychiatric medication development trials could be much better for patients both in trials and in treatment
The standard randomized parallel-group design leaves a crucial causal ambiguity. If 60% of those treated with medication have substantial improvements, while only 30% of those on placebo improve (assuming statistical significance), then in about half of those who seemed to have a direct drug benefit, the drug was actually not required. Identifying individuals who actually require medication to improve and maintain their gains remains obscure. Therefore, attempts to determine how a drug brought about its benefits by studying those who improved during drug treatment are handicapped by study of a causally heterogeneous mixture.
…an alternative design would be to initially and openly treat all patients with the putative medication, titrating for the individual’s optimal dose, until it is clear if the patient was not a treatment responder. These subjects would leave the trial. Apparent responders would be maintained on medication for a period, but then randomly, and in double-blind fashion, switched to placebo or remain on medication. All patients would be followed independently and closely, blind to treatment status, for defined signs of worsening. At a predetermined level of modest worsening, double-blind medication retreatment would start. A worsening rate higher in the placebo-substituted group than in the medication-maintained group would provide clear evidence of medication efficacy. Those individuals who worsened on slow placebo substitution and then improved on medication re-treatment are very likely specific drug responders. Those who switched to placebo and nevertheless continued to do well would be far less likely to be specific medication responders.
To summarize, this design would determine individuals very likely to be medication-specific responders, very likely non-specific responders, and non-responders.
Other practical benefits are that all patients initially receive active treatment. This fosters recruitment, since many patients will not risk being initially assigned to placebo. In addition, patients will learn if medication is necessary for them to remit or that they have sufficient resources.
In fact, academic investigators have successfully used this design.
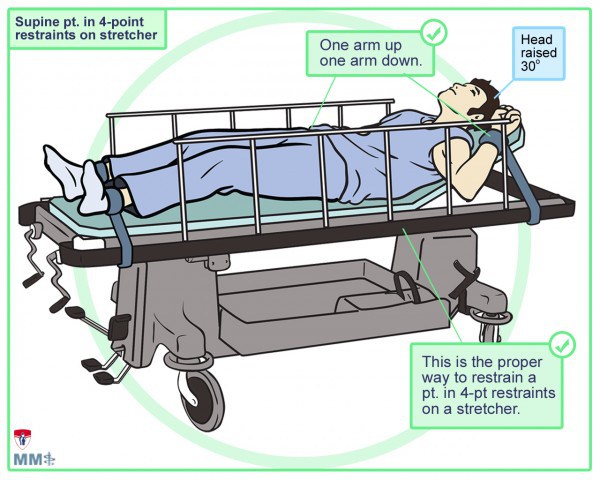
- Weingart, Scott. “Podcast 060 – On Human Bondage and the Art of the Chemical Takedown.” org, 13 Nov. 2011, emcrit.org/podcasts/human-bondage-chemical-takedown/. Accessed 25 Feb. 2017.
- Klein, Donald F., and Ira D. Glick. “Industry withdrawal from psychiatric medication development.” Revista Brasileira de Psiquiatria 36.3 (2014): 259-261.