Cognitive therapy neural networks are changed bottom-up in antidepressant therapy and top-down in cognitive therapy
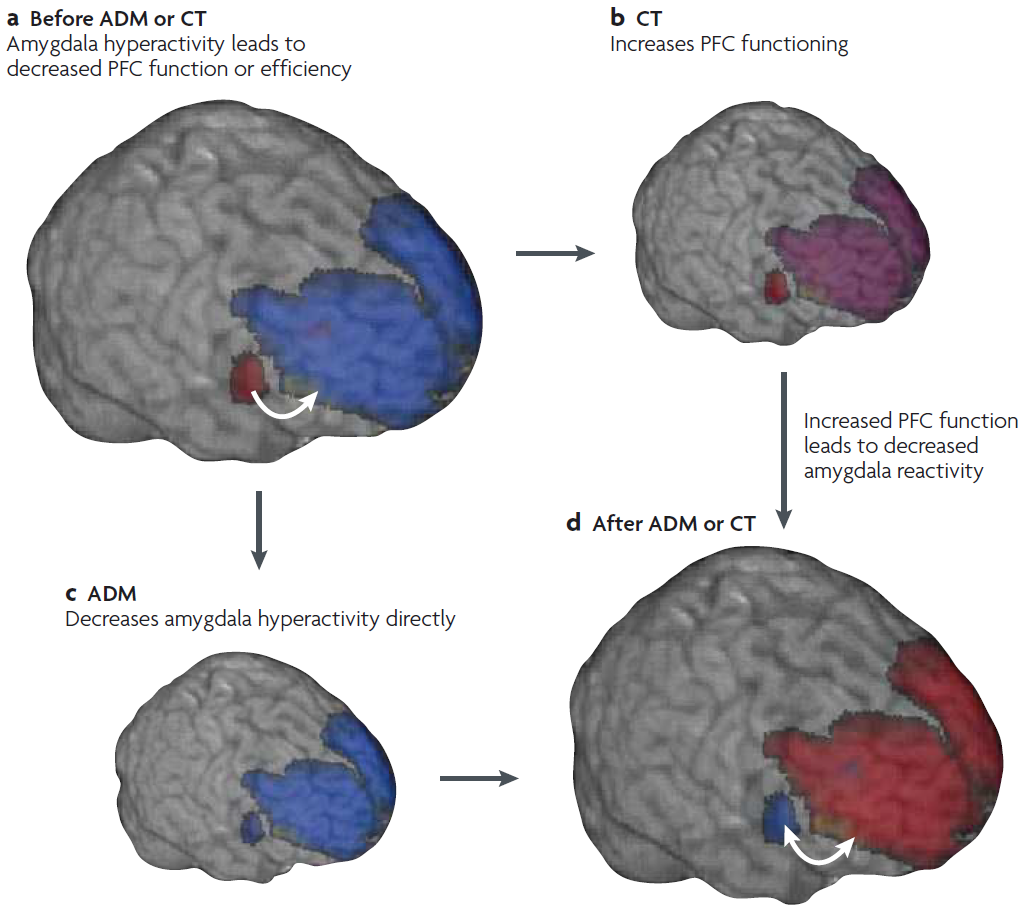
Hypothetical time course of the changes to amygdala and prefrontal function that are associated with antidepressant medication and cognitive therapy.
a | During acute depression, amygdala activity is increased (red) and prefrontal activity is decreased (blue) relative to activity in these regions in healthy individuals.
b | Cognitive therapy (CT) effectively exercises the prefrontal cortex (PFC), yielding increased inhibitory function of this region.
c | Antidepressant medication (ADM) targets amygdala function more directly, decreasing its activity.
d | After ADM or CT, amygdala function is decreased and prefrontal function is increased. The double-headed arrow between the amygdala and the PFC represents the bidirectional homeostatic influences that are believed to operate healthy individuals.[1]
Cognitive therapy neural networks –
– work together (along the black lines) to produce depressed symptoms
– feed back the results (along the gray line) to generate depressed symptoms in the future
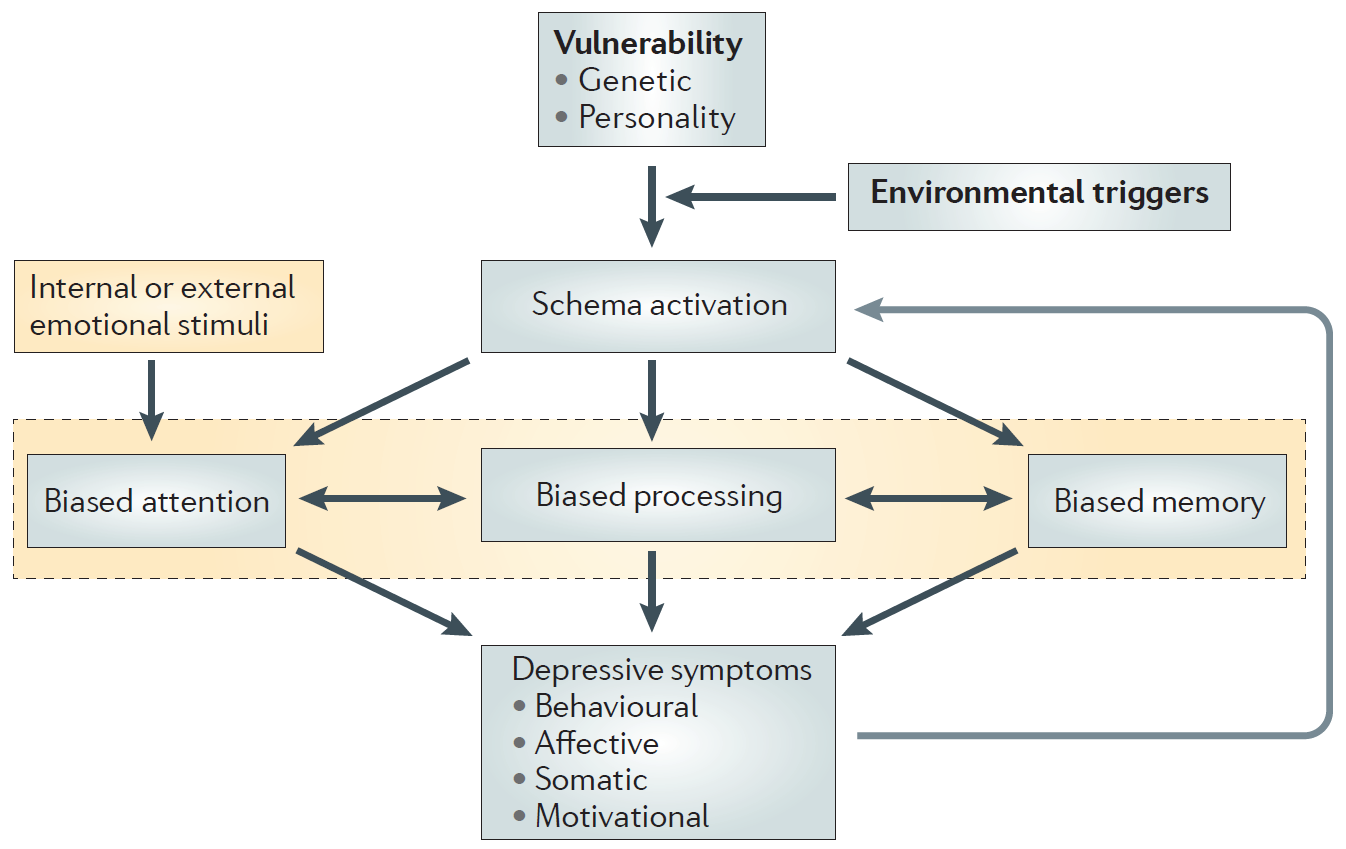
Information processing in the cognitive model of depression.
- Activation of depressive self-referential schemas by environmental triggers in a vulnerable individual is both the initial and penultimate element of the cognitive model.
- The initial activation of a schema triggers biased attention, biased processing and biased memory for emotional internal or external stimuli.
- As a result, incoming information is filtered so that schema-consistent elements in the environment are over-represented.
- The resulting presence of depressive symptoms then reinforces the self-referential schema (shown by a grey arrow), which further strengthens the individual’s belief in its depressive elements.
- This sequence triggers the onset and then maintenance of depressive symptoms.[2]
Untreated cognitive therapy neural networks take negative schema information and fan it out, and add in overgeneral negative information
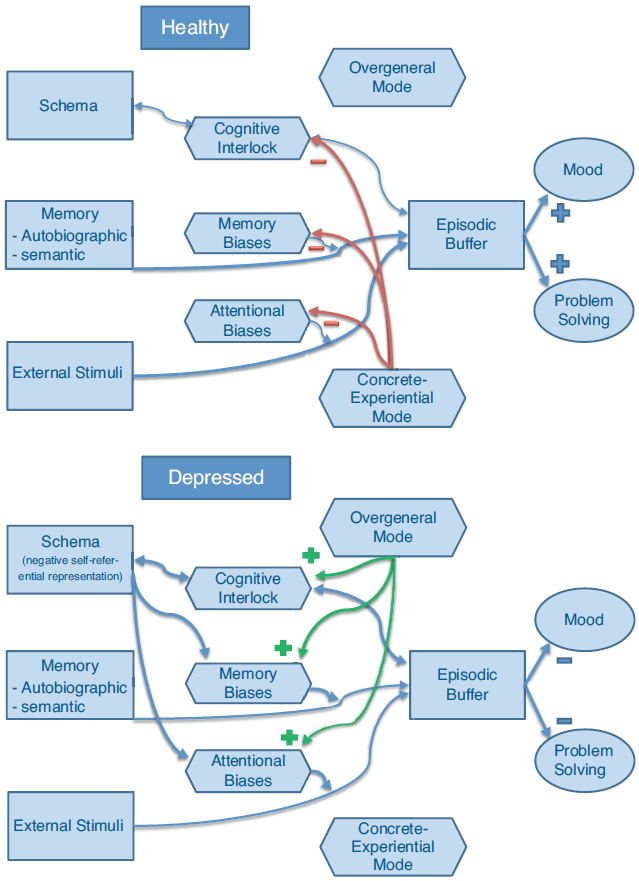
Cognitive functioning in a healthy (a) or depressed (b) individual.
- In a depressed individual, a negative self-schema and an over-general mode of processing concur to automatically prime and activate information that is congruent with the negative self-schema, via a cognitive interlock (resulting in rumination), biased memory and attention.
- In a healthy individual, a concrete mode of processing counteracts these automatic activations.
Cognitive therapy neural networks information flow (in the diagrams above) maps directly to neural regions (in the pictures below)
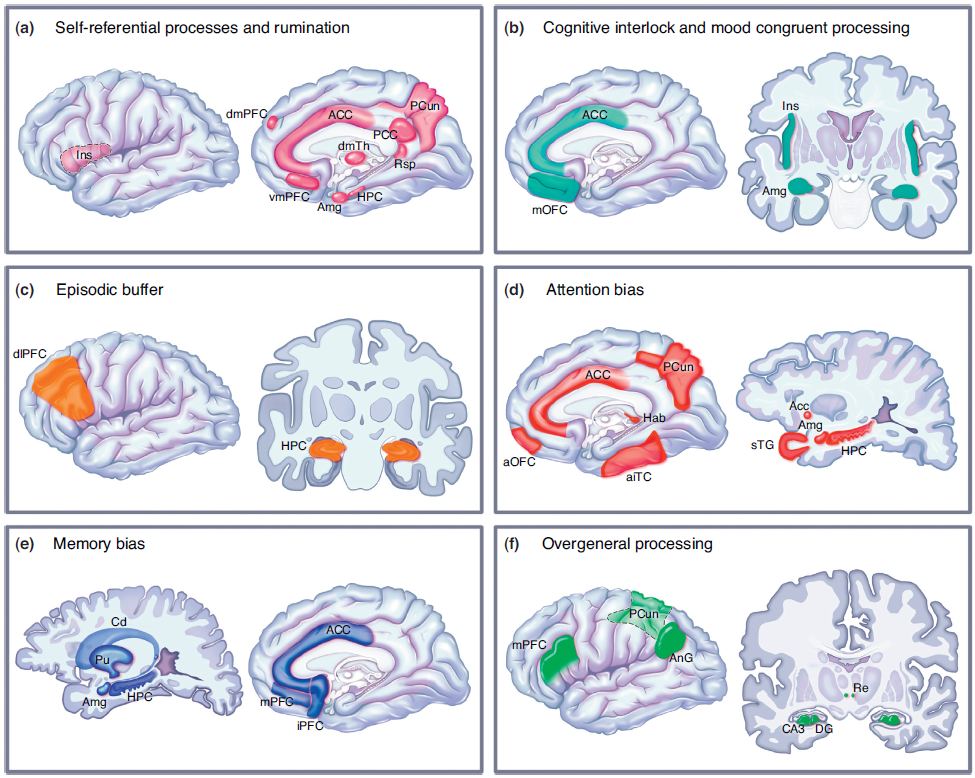
Brain networks involved in
(a) self-referential processes and rumination,
(b) cognitive interlock and mood congruent processing,
(c) episodic buffer,
(d) attention bias,
(e) memory bias,
(f) overgeneral processing.
dmPC: dorsomedial prefrontal cortex,
vmPFC: ventromedial prefrontal cortex,
mPFC: medial prefrontal cortex,
iPFC: inferior prefrontal cortex,
mOFC: medial orbitofrontal cortex,
aOFC: anterior orbitofrontal cortex,
dlPFC: dorsolateral prefrontal cortex,
aITC: anterior inferotemporal cortex,
STG: superior temporal gyrus,
AnG: angular gyrus,
Ins: insula,
ACC: anterior cingulate cortex,
PCC: posterior cingulate cortex,
PCun: precuneus,
Rsp: retrosplenial cortex,
dmTh: dorsomedial thalamus,
HPC: hippocampus,
Amy: amygdala,
Hab: habenula,
Acc: nucleus accumbens,
Cd: caudate,
Pu: putamen,
Re: nucleus reuniens,
DG dentate gyrus of the hippocampus.[3]
- DeRubeis, Robert J., Greg J. Siegle, and Steven D. Hollon. “Cognitive therapy versus medication for depression: treatment outcomes and neural mechanisms.” Nature Reviews Neuroscience 9.10 (2008): 788-796.
- Disner, Seth G., et al. “Neural mechanisms of the cognitive model of depression.” Nature Reviews Neuroscience 12.8 (2011): 467-477.
- Belzung, Catherine, Paul Willner, and Pierre Philippot. “Depression: from psychopathology to pathophysiology.” Current opinion in neurobiology 30 (2015): 24-30.